Treatment of Leukimia
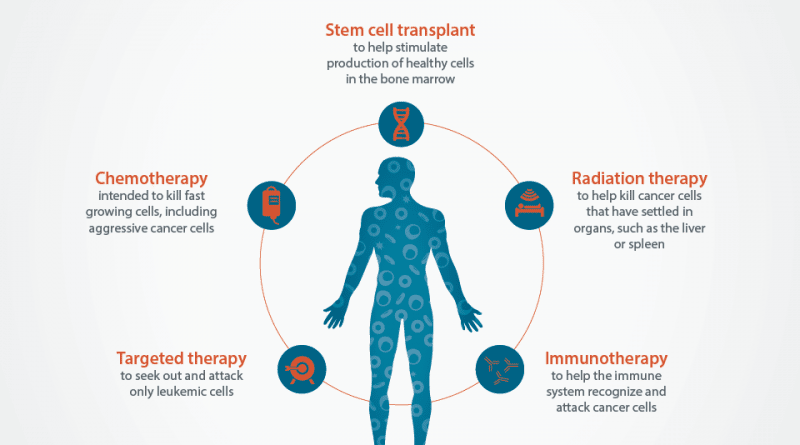
Treatment of leukemia depends on the type and level of disease and is tailored for each patient. In general, chemotherapy-the use of drugs that kill rapidly dividing cells is the main treatment for acute or chronic leukemia. In acute leukemia, intensive chemotherapy and the use of some drugs, either simultaneously or sequentially, kill the leukemia cells as possible. Antibiotics and transfusions of red blood cells and platelets help the blood to maintain a low number of patients who are dangerous because they received intensive chemotherapy.
Sometimes radiation is used to shrink the collection of leukemia cells that accumulate in various parts of the body, such as the lining of the brain and spinal cord in acute lymphocytic leukemia, or the lymph nodes in chronic lymphocytic leukemia. If not treated, a collection of cells on the lining of the brain and spinal cord can cause headaches, blurred vision, and confusion, and elsewhere in the body can cause swelling and pain from the affected area.
Especially in younger patients, if doctors determine that chemotherapy alone is not likely to succeed or if the patient relapse after chemotherapy, allogeneic (genetically different) stem cell transplants can be performed. In this procedure, very intense total body irradiation or high-dose chemotherapy, or both were used. Chemotherapy and radiation are designed to destroy all the leukemia cells in the body of the patient, but this treatment also destroys the blood-forming system in the bone marrow of patients.
For this reason, the healthy stem cells, bone marrow cells that allow the formation of long-term blood, then be inserted into patients to replace the blood-forming system. Stem cells must come from immunologically suitable donors, usually siblings, but if your game is not available, sometimes an unrelated donor may be sought. The latter can be identified from the database of voluntary donors. This database can be searched for people with matching tissue types that are identical or very close.
Previously, stem cells can only be transplanted from donor bone marrow. This procedure is known as a bone marrow transplant. Recent advances now enable the recovery of stem cells from blood, or the placenta and umbilical cord blood (“cord blood”) after giving birth to newborns, making the transplant procedure much simpler and less risky for the donor. Cord-blood stem cells are frozen, stored in a bank “,” and can be used later for patients who need them.
The number of stem cells in this sample may not be sufficient for larger adults and is most commonly used for children or smaller adults who need transplants and need donors, or unrelated matches.
An unexpected effect of allogeneic stem cell transplant is what is known as the effect of graft-versus leukemia. Immune cells recognize the donor antigen in small tissue types (proteins that produce antibodies) that are incompatible with the recipient. This donor’s immune cells attack the recipient’s network, including leukemia cells and normal tissue. The attack on normal tissue recipients is a disease called graft-versus-host.
This attack can be acute or chronic, and very mild or very severe. This is a serious complication that is not desirable from allogeneic stem cell transplantation. Graft-versus-leukemia-cells, on the other hand, are the desired effect and are responsible in part for some beneficial effects of transplantation, especially in patients who received transplants for the treatment of acute or chronic myelocytic leukemia.
Transplantation is the most effective in children and young adults; for older adults is often too dangerous a procedure to apply. A transplant approach called non-myeloablative stem cells is being tested on older patients. Here a very mild pretreatment with chemotherapy or radiation is used, whereas the anti-immune therapy is based on the immune system to prevent recipients from stem cells rejecting donors. Stock graft-versus-leukemia who relied on as a substitute for intensive therapy given before transplantation for leukemia standards.
Immunotherapy is a promising new approach to treating leukemia. With this technique, highly specific molecules known as monoclonal antibodies are made in the laboratory to the target molecule on the surface of leukemia cells. The antibody itself may kill leukemia cells, or radioactive substances or toxic cells attached to the antibody can kill leukemia cells when injected intravenously into the patient. This method provides an easy way to deliver immediate radioactive or toxic substances into the leukemia cells, which may kill cells with minimal effect on healthy cells.
The objective in the treatment of acute leukemia is to kill leukemia cells is sufficient to produce remission, which means that the production of red blood cells is no longer suppressed, blood cell counts returned to normal, and patient symptoms decreased. At that stage, further therapy is used to try to extend the reach of remission or cure. Approximately 80 percent of children with acute lymphocytic leukemia can be cured. The cure rate of acute myelocytic leukemia is estimated at around 40 percent in children but much lower in adults depending on their age. Because most patients are more than 65 years when they develop the disease, treatment is rare.
In chronic leukemia, the cure is rare, but the current chemotherapy regimens have improved survival in patients with an average of about three years to more than six years. chronic lymphocytic leukemia in the lazy form may not require treatment and may not progress or a serious health consequences for patients. In patients with active or progressive disease, new drugs and types of available monoclonal antibodies to treat the disease.
In chronic myelocytic leukemia, dramatic advances in therapy involve the introduction of drugs that specifically target leukemia causing changes in bone marrow cells. The introduction of this treatment has been projected to increase survival for more than a decade on average. Young patients with diseases that have an appropriate stem cell donor can be cured by stem cell transplantation.